Which countries are fighting the toughest battles against sexually transmitted infections (STIs)? Finding out where STIs are most common helps us understand the health challenges these countries face. It’s the first step towards finding solutions.
Every day, over 1 million new cases of STIs pop up worldwide1. In 2020, the World Health Organization (WHO) found 374 million new cases of 4 STIs: chlamydia, gonorrhea, syphilis, and trichomoniasis2. Also, about 300 million women got an HPV infection, which can lead to cervical cancer1. These numbers show how STIs affect global health.
Key Takeaways
- The global prevalence of sexually transmitted infections (STIs) is alarmingly high, with over 1 million new cases acquired every day.
- In 2020, the World Health Organization (WHO) estimated 374 million new infections with 4 curable STIs: chlamydia, gonorrhea, syphilis, and trichomoniasis.
- An estimated 300 million women have an HPV infection, the primary cause of cervical cancer.
- High STI rates have a significant impact on global sexual and reproductive health.
- Understanding the geographical distribution of STI prevalence is crucial for developing targeted prevention and control strategies.
The Scope of STIs Worldwide
Every year, a staggering 374 million new sexually transmitted infections (STIs) occur worldwide3. Chlamydia, gonorrhea, syphilis, and trichomoniasis lead the pack in new cases3. In 2016, about 490 million people had genital herpes, and by 2022, around 254 million had hepatitis B3.
Staggering Global STI Statistics
The World Health Organization (WHO) says over 1 million new STIs are caught every day globally4. This is a big public health issue. STI rates are going up in places like the United States and the United Kingdom4. This shows how important it is to watch these trends closely.
High-Burden STIs and Their Impact
Herpes, gonorrhea, and syphilis make getting HIV more likely3. Hepatitis B led to over 1 million deaths in 2022, mostly from liver problems and liver cancer3. Gonorrhea and chlamydia also cause a lot of pelvic inflammatory disease and infertility in women3.
Dealing with the global STI problem is a big challenge for public health3. High-burden STIs can increase the risk of getting HIV, passing STIs to babies, causing infertility, and even cancer3.
Countires with the most STDs
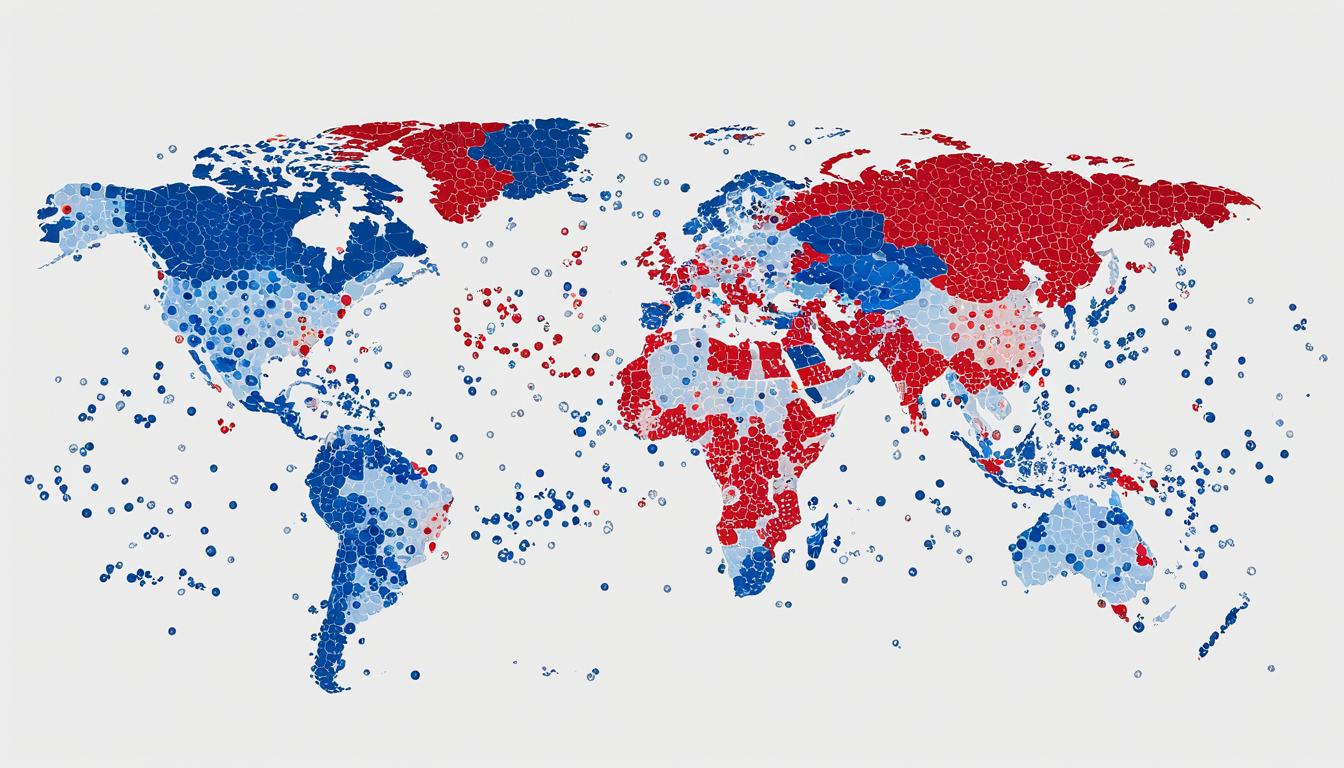
Sexually transmitted infections (STIs) are a big concern worldwide. Some countries and regions have a lot more cases than others. South Africa, Namibia, Botswana, Swaziland, and Lesotho in Africa, and some Eastern European countries, have the highest STI rates5.
These high rates are due to many factors. Societal norms, economic differences, limited healthcare access, and poor prevention efforts play a big part5.
In Europe, chlamydia is often the most common STD in the north and east. Hepatitis C is most common in central Europe5. Spain, France, and Italy have more new HIV cases than other STDs5. Iceland leads in chlamydia, hepatitis B, and hepatitis C infections. Russia has the most STD infections in Europe5.
The United States also struggles with STDs. Washington D.C. has the highest HIV, syphilis, and gonorrhea rates in the US5. Nearby states and the Deep South also have high rates5. Chlamydia cases have risen over the years, but gonorrhea has decreased since 19845. Washington D.C.’s gonorrhea rates are much higher than any US state5.
Worldwide, the World Health Organization says over a million new curable STD infections happen every day6. Countries like Eswatini, Lesotho, Botswana, South Africa, and Namibia have the highest HIV rates6. The US has the third-highest gonorrhea rate in the developed world6. The most common STD globally is Human Papillomavirus (HPV), with over 600 million cases worldwide and 20 million in the US6.
| Top 10 Countries with the Highest Rates of HIV (per 100K population) |
|---|
| 1. Eswatini: 18697.64 |
| 2. Lesotho: 17883.06 |
| 3. Botswana: 15007.47 |
| 4. South Africa: 14250.79 |
| 5. Namibia: 8545.85 |
| 6. Zimbabwe: 8174.72 |
| 7. Mozambique: 7976.64 |
| 8. Zambia: 6710.91 |
| 9. Malawi: 5456.75 |
| 10. Equatorial Guinea: 5027.23 |
“The District’s Department of Health acknowledged struggling with an epidemic of chlamydia, gonorrhea, hepatitis, and HIV.”5
Major Contributors to STI Prevalence
Sexually transmitted infections (STIs) are influenced by many factors. High-risk STD regions face deep stigma around sex and STIs. This makes people less likely to get tested and treated.
Sociocultural factors of STDs like poor sex education and taboos make things worse. Economic factors of STDs also matter a lot. Poverty, lack of healthcare access, and money issues stop people from getting tested and treated, especially in poor areas.
Sociocultural and Economic Determinants
Young people, aged 15 to 24, get half of all new STIs, even though they’re only 25% of those who are active in sex7. Women face more serious STI issues than men. They’re more likely to get pelvic inflammatory disease, ectopic pregnancy, infertility, and chronic pelvic pain7.
Some racial and ethnic groups, like African American, Hispanic, and American Indian/Alaska Native, get more STIs than whites7. This is often because they live in poverty. They have less healthcare access, avoid doctor visits, and live in areas with more STIs7.
Using drugs also raises the risk of getting STIs. It can lead to risky sex behaviors in communities7. Stigma and discomfort talking about sexual health spread STIs in the U.S7..
| Sociocultural Factors | Economic Factors |
|---|---|
|
|
To fight STIs, we must address the sociocultural factors of STDs and economic factors of STDs. We need better healthcare systems, new ways to talk about health, and programs that tackle barriers and health gaps78.
Consequences of Untreated STIs
Sexually transmitted infections (STIs) can have severe consequences if left untreated. Chlamydia and gonorrhea can cause pelvic inflammatory disease and infertility in women if not treated9. Viral STIs like HIV, genital herpes simplex virus (HSV), and human papillomavirus (HPV) can affect a person for life9.
Impact on Reproductive Health
Untreated STIs affect more than just the person infected. They can harm reproductive health, the health of mothers and babies, and the health of communities10. Syphilis can cause serious problems during pregnancy, like stillbirth and congenital syphilis10. It’s important to diagnose and treat STIs quickly to protect reproductive health10.
Risks of HIV Acquisition
STIs like herpes, syphilis, and gonorrhea can make getting HIV more likely, which worsens the HIV/AIDS epidemic9. People with untreated STIs are more at risk of getting HIV. This shows why we need to prevent and control STIs10.
| Viral STIs with Limited Treatment Options | Available Vaccines | Lifelong Infections and Treatments |
|---|---|---|
| HIV, genital herpes simplex virus (HSV), viral hepatitis B, human papillomavirus (HPV), and human T-lymphotropic virus type 1 (HTLV-1) | Hepatitis B, HPV | HIV and HSV (treatments exist to suppress, but no cures) |
“The World Health Organization (WHO) highlights the global concern regarding sexually transmitted infections (STIs) and offers guidelines and strategies for HIV, viral hepatitis, and STIs for various periods.”
Untreated STIs can have serious effects on health, including reproductive health, the health of mothers and babies, and the risk of HIV910. It’s important to diagnose, treat, and prevent STIs to protect health910.
Prevention Strategies for STIs
Effective prevention strategies are key to fighting the global STI epidemic. Using condoms correctly and consistently is a top way to protect against STIs, including HIV11. Also, safe sex practices like having fewer partners and avoiding risky actions can help stop STIs from spreading11.
Condom Use and Safe Sexual Practices
Teaching about sex, reaching out to people, and making STI tests and treatments easy to get are important for preventing STIs1112. Using polyurethane condoms also protects against STIs and HIV, just like latex ones, and works with any lubricant.11
Studies show that in relationships where both partners have HIV and use condoms, the HIV-negative partner is 71%–80% less likely to get HIV.11 Also, condoms might break more often during anal sex.11
- HPV vaccine is advised up to age 26 for those not vaccinated before11.
- In the U.S., about two condoms break out of 100.11
- Internal condoms also protect against STIs.11
- Diaphragms help prevent cervical infections like gonorrhea and chlamydia.11
Methods that don’t use barriers don’t protect against HIV or STIs.11 Also, topical microbicides and spermicides don’t stop HIV, and some increase the risk of infections.11
“Promoting safe sex and easy access to STI tests and treatments is key to fighting the STI epidemic.”
By using condoms, practicing safe sex, and making health services available, we can lessen the impact of STIs worldwide1112.
Vaccination Against Viral STIs
Vaccines have made a big leap in preventing sexually transmitted infections (STIs), especially for viral ones. For example, vaccines for hepatitis B13 and human papillomavirus (HPV) are safe and work well. They can stop these viral STIs and prevent serious health issues like liver disease and cervical cancer13. Scientists are also working hard to make vaccines for other STIs, like genital herpes, to fight the global STI problem14.
The HPV vaccine has changed the game in fighting viral STIs. In 2006, the U.S. FDA approved Gardasil (HPV4) for four types of HPV. Then, in 2009, Cervarix (HPV2) was approved for two types of HPV13. In 2014, the nine-valent vaccine (HPV9, Gardasil 9) was approved, covering more HPV strains13. Research shows that up to 95% of people who get the hepatitis B virus can fully recover and don’t stay infected, thanks to vaccines13.
Even with these advances, making vaccines for other viral STIs is still a challenge. For example, genital herpes vaccines haven’t been approved yet. A 2010 trial for a herpes vaccine didn’t show it was effective13. Only three HIV vaccines have been tested in real-world trials since 1983, showing we need more research and innovation13.
Creating and using STD vaccines, especially for viral infections, could greatly reduce STIs and their health effects worldwide14. As research and trials go on, we’ll likely see more progress in preventing viral STIs with vaccines15.
Diagnostic Challenges in STI Testing
Diagnosing sexually transmitted infections (STIs) can be tough because many don’t show symptoms16. In rich countries, advanced tests are common, but in poor ones, they’re rare16. This means people might not get tested or treated on time, especially in places with less resources.
Availability of Rapid Tests
There’s hope, though. Rapid tests for STIs like syphilis and HIV work well in poor areas16. They give results fast, helping doctors start treatment and tell others who might be infected16. But, we need to make these tests cheaper and more available for infections like chlamydia and gonorrhea16.
Testing for STDs faces more hurdles because many infections don’t show up right away16. Also, bacteria like Neisseria gonorrhoeae are becoming resistant to antibiotics, making things harder16. This calls for global action to fight this problem16.
Healthcare workers and health officials are trying hard to make sure people can get quick and accurate tests16. They want to help everyone stay healthy in what they do sexually.
“Expanding access to rapid STD tests is crucial for early detection and treatment of sexually transmitted infections, especially in resource-limited settings.”
Treatment Options and Antimicrobial Resistance
Many sexually transmitted infections (STIs) like chlamydia, gonorrhea, syphilis, and trichomoniasis can be cured. They often need just one dose of antibiotics17. But, the rise of antibiotic resistance, especially in gonorrhea, has made treatment harder. This is a big public health issue18.
Gonorrhea, caused by Neisseria gonorrhoeae, affects millions every year. It’s a big concern because it’s becoming resistant to many antibiotics1918. Now, ceftriaxone is the only antibiotic left for treating gonorrhea in most places18.
Antibiotic resistance isn’t just a problem for gonorrhea. Mycoplasma genitalium, another STI, is also becoming resistant to treatments1918. In the U.S., trichomoniasis treatments are also showing resistance18.
We need to tackle antibiotic resistance in STIs to manage and control diseases. We must keep an eye on how bacteria are changing and find new antibiotics18. The World Health Organization has a plan to fight gonorrhea and track antibiotic resistance18.
In short, while we have treatments for many STIs, antibiotic resistance is a big problem. We must keep watching and finding new antibiotics to manage STIs effectively191718.
Syndromic Management of STIs
In places with limited resources, doctors often use syndromic management to diagnose and treat STIs. This method relies on symptoms to guide treatment, skipping lab tests20. It allows for quick treatment but might lead to over-treatment and missed diagnoses, as many STIs don’t show symptoms20. The World Health Organization suggests using lab tests when possible to improve this method20.
Treating Sexual Partners
Treating the sexual partners of those with STIs is key to stopping the spread of infection and preventing new cases20. Research shows that a test called Xpert CT/NG is effective in South Africa for diagnosing chlamydia and gonorrhea21. Another test, the GeneXpert system, can also be used for STI testing in South Africa21.
In the UK, the USA, and Australia, a method called expedited partner therapy (EPT) was used for chlamydia. It cut the risk of reinfection in women by 20%–29%21. Yet, a study in rural KwaZulu-Natal found that only 13.1% of people got proper treatment for STIs through syndromic services21. This shows we need better ways to treat partners for syndromic STD management and partner treatment for STDs.

“Over 25% of women at the time of acute HIV infection in South Africa had at least one laboratory-diagnosed STI, indicating a high prevalence of STIs in this population.”21
Just looking at symptoms missed 88% of STIs in women, showing the need for tests in HIV and STI care21. Research funded by the National Institute of Health and the South African Medical Research Council looked into how better STI care affects genital health and HIV risk21.
In conclusion, managing STIs through syndromic methods and treating partners is vital to stop disease spread and prevent reinfection. But, its limits show we need better tests and services for effective management and control of these infections2021.
Barriers to STI Prevention and Control
Despite efforts to fight sexually transmitted infections (STIs), big hurdles still slow down progress. Lack of public awareness about STIs and their dangers, plus the stigma around them, are big problems22.
Many people don’t know the signs of STIs or when to get help23. Doctors also struggle to get the right training and support to handle STIs well, making things worse23.
We need to tackle these big issues with strong public education campaigns, efforts to reduce stigma, and specific actions. This will help improve STI prevention and control for everyone23. Giving people the right info and support, in a supportive and inclusive society, will make STI control efforts work better24.
The rise in STIs worldwide shows we must act fast to fix these problems24. We need to focus on groups at higher risk, like men who have sex with men, transgender women, and teens, to lessen their STI load2423.
“Addressing the systemic barriers to STI prevention and control is crucial for improving public health outcomes and promoting sexual and reproductive well-being globally.”
Behavior Change and Public Awareness
Changing behavior for the long term is hard in fighting STIs. We need to teach people to use condoms and have fewer partners to stay safe23.
Good sexuality education in schools and community programs is key to getting people to know the risks and behave responsibly23. Putting money into these efforts can help stop STIs from spreading and create a culture of prevention22.
By getting past these STI prevention and control barriers, we can make a better future. People will be able to make smart choices about their sexual health242322.
Strengthening Health Services for STIs
Improving healthcare for sexually transmitted infections (STIs) is key to tackling these diseases worldwide. But, many low- and middle-income countries struggle with limited resources and training issues25.
To fight the STI epidemic, we need to make healthcare better. This means adding STI services to primary care, making care more accessible, and increasing testing at clinics26.
- Adding STI services to primary care helps reach more people, especially in hard-to-reach areas25.
- Making care more focused on the patient’s needs can lower the barriers to getting tested and treated25.
- Using rapid tests at clinics can speed up treatment, especially for high-risk groups25.
Improving healthcare’s ability to handle STIs is a big step towards reducing these infections and better health outcomes263.
“Investing in strengthening STI healthcare services is a critical component of the global effort to end the epidemics of sexually transmitted infections by 2030.”
The World Health Organization has a plan to fight HIV, Hepatitis, and STIs. It sets global goals, monitors resistance to gonorrhea, and leads in STI research3.
WHO’s Global Strategy on STIs
The World Health Organization (WHO) has created a detailed Global Health Sector Strategy on HIV, hepatitis, and sexually transmitted infections (STIs) for27. This plan highlights key areas for global STD control. It aims to help countries fight the growing health issue of sexually transmitted infections28.
Key Areas of Focus
The WHO’s strategy on STIs focuses on several key areas:
- Supporting countries in making and using STI plans and policies
- Improving STI surveillance to understand disease trends and improve programs29
- Addressing antimicrobial resistance, a big threat to STI treatment28
- Increasing access to prevention, testing, and treatment for STIs, especially for vulnerable groups27
The WHO also leads global research on STIs. It aims to develop new tests, vaccines, and treatments to fight this health issue29.
“The WHO Global STI Strategy aims to save lives, enhance health outcomes, and improve the health of millions. It recommends key actions for countries, including surveillance improvement, prevention, diagnosis, patient care, and reaching vulnerable groups.”
This strategy focuses on key areas to help countries strengthen their STI control efforts. It aims to move towards the 2030 global targets29.
Supporting National STI Programs
Effective national STI programs are key to fighting the global STI epidemic at the country level30. In 2022, the CDC reported over 2.5 million cases of syphilis, gonorrhea, and chlamydia in the U.S30.. Syphilis cases have jumped by 80 percent in five years, and congenital syphilis cases have soared by 937 percent in a decade30.
The World Health Organization (WHO) helps by offering technical advice and promoting global standards31. It also aids in making strategic plans and guidelines31. Strengthening healthcare systems and improving STI service access are key31. Global and national efforts are vital for controlling STIs worldwide.
The STI National Strategic Plan in the U.S. has five main goals31. These goals aim to prevent new STIs, improve health outcomes, speed up research, reduce disparities, and coordinate efforts31. The plan focuses on chlamydia, gonorrhea, syphilis, and HPV as major STIs affecting public health31.
- The plan tackles stigma, discrimination, and health determinants to address rising STI rates31.
- It sets progress indicators, baseline measurements, and annual targets through 203031.
- Federal partners will create an implementation plan to support the STI Plan goals, ensuring transparency and accountability31.
Effective national STI programs, backed by global efforts, are vital for tackling the growing STI public health challenge.
Conclusion
Sexually transmitted infections (STIs) are a huge problem worldwide, with over 1 million new cases every day32. From 1990 to 2019, the number of STI cases jumped by 58.15%, reaching 769.85 million32. Infections like chlamydia, gonorrhea, and syphilis affect people’s health all over the world3334.
In the 1990s, North America and western Europe saw 30 million cases of curable STIs each year34. Eastern Europe and Central Asia had another 18 million cases. The World Health Organization found 333 million new cases of curable STDs in 1995. This included 62 million gonorrhea cases, 89 million chlamydia cases, 12 million syphilis cases, and 170 million trichomoniasis cases.
To fight this health issue, we need to improve prevention, testing, treatment, and address social and economic factors333432. We must work together worldwide, following the WHO’s plan, to stop STIs and better health outcomes.
The global STD situation is alarming, with over 1 million new cases daily32. To control STDs, we need a full approach. This includes global coordination and the WHO’s guidance.
FAQ
What is the global prevalence of sexually transmitted infections (STIs)?
Every day, over 1 million new cases of STIs are reported worldwide. In 2020, the World Health Organization found 374 million new cases of four curable STIs. These include chlamydia, gonorrhea, syphilis, and trichomoniasis. Also, 300 million women have an HPV infection, linked to cervical cancer.
What are the high-burden STIs globally?
High-burden STIs include chlamydia, gonorrhea, syphilis, trichomoniasis, genital herpes, and hepatitis B. These infections can increase the risk of HIV, cause infertility, and lead to cancer.
Which countries have the highest reported rates of STIs?
Countries like South Africa, Namibia, Botswana, Swaziland, and Lesotho have high STI rates. Factors include cultural norms, economic issues, limited healthcare access, and prevention efforts.
What factors contribute to the high prevalence of STIs?
Sociocultural and economic factors play a big role in STI rates. Stigma around STIs and sexuality can stop people from getting tested. Poverty and limited healthcare access also add to the problem.
What are the consequences of untreated STIs?
Untreated STIs can cause serious health issues. Chlamydia and gonorrhea can lead to pelvic inflammatory disease and infertility. They can also raise the risk of getting HIV, making the HIV/AIDS problem worse.
What are the key prevention strategies for STIs?
Key strategies include using condoms correctly and safely, promoting safe sex, and giving comprehensive sex education. Targeted outreach and increasing access to testing and treatment are also important.
How have vaccines contributed to STI prevention?
Vaccines for hepatitis B and HPV prevent these viral STIs and their complications. Research is ongoing for vaccines against other STIs, like genital herpes.
What are the challenges in STI diagnosis?
Diagnosing STIs can be tough because many don’t show symptoms. In low-income areas, advanced tests are rare. This makes getting timely treatment hard.
What are the challenges in STI treatment?
Treating STIs is hard because of antibiotic resistance, especially in gonorrhea. This reduces treatment options. Watching antibiotic resistance and finding new treatments is key to managing STIs well.
What is syndromic management of STIs?
In places with limited resources, doctors use syndromic management for STIs. They treat based on symptoms without lab tests. This can lead to over-treatment and missed diagnoses, since many STIs don’t show symptoms.
What are the barriers to STI prevention and control?
Barriers include lack of awareness, stigma, and making lasting behavior changes. Many don’t know how to spot STI symptoms or get timely care. Health workers might not know how to manage STIs well.
How can healthcare services be strengthened for STI prevention and control?
Healthcare services need to improve for STI prevention and treatment. This means adding STI care to primary healthcare, making care more accessible, and using point-of-care testing to boost the healthcare system’s response to STIs.
What is the World Health Organization’s (WHO) global strategy on STIs?
The WHO has a global strategy on HIV, hepatitis, and STIs for 2022-2030. It focuses on supporting countries, improving STI surveillance, fighting antibiotic resistance, and increasing prevention, testing, and treatment services.
How do national STI programs support the global effort?
National STI programs are vital for tackling the STI epidemic at home. The WHO helps by offering technical support, promoting global standards, and helping with strategic plans. Improving healthcare systems and access to STI services is crucial.
Source Links
- Global perspectives on the burden of sexually transmitted diseases: A narrative review – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11098264/
- Global and regional STI estimates – https://www.who.int/data/gho/data/themes/topics/global-and-regional-sti-estimates
- Sexually transmitted infections (STIs) – https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
- WHO releases new guidance to improve testing and diagnosis of sexually transmitted infections – https://www.who.int/news/item/24-07-2023-who-releases-new-guidance-to-improve-testing-and-diagnosis-of-sexually-transmitted-infections
- Prevalence of STDs Across the United States and Europe – https://onlinedoctor.superdrug.com/std-us-eu.html
- STD Rates by Country 2024 – https://worldpopulationreview.com/country-rankings/std-rates-by-country
- Sexually Transmitted Infections Workgroup – Healthy People 2030 – https://health.gov/healthypeople/about/workgroups/sexually-transmitted-infections-workgroup
- Estimating prevalence and incidence of sexually transmitted infections among South African Women: implications of combined impacts of risk factors – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8032503/
- Sexually transmitted infections (STIs) – https://www.who.int/health-topics/sexually-transmitted-infections
- Sexually Transmitted Infections | Travelers’ Health – https://wwwnc.cdc.gov/travel/page/std
- Primary Prevention Methods – https://www.cdc.gov/std/treatment-guidelines/clinical-primary.htm
- Prevention strategies for sexually transmitted infections, HIV, and viral hepatitis in Europe – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10625023/
- Sexually Transmitted Infections – https://historyofvaccines.org/diseases/sexually-transmitted-infections
- Future prospects for new vaccines against sexually transmitted infections – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5325242/
- Priorities for sexually transmitted infection vaccine research and development: Results from a survey of global leaders and representatives – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8356130/
- Diagnosing sexually transmitted infections in resource‐constrained settings: challenges and ways forward – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6715950/
- Growing antibiotic resistance forces updates to recommended treatment for sexually transmitted infections – https://www.who.int/news/item/30-08-2016-growing-antibiotic-resistance-forces-updates-to-recommended-treatment-for-sexually-transmitted-infections
- Addressing antimicrobial resistance in STIs – https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/stis/treatment/addressing-amr-in-stis
- Rising antimicrobial resistance in STIs: A call for global action – https://www.news-medical.net/news/20240321/Rising-antimicrobial-resistance-in-STIs-A-call-for-global-action.aspx
- Syndromic Management of Sexually Transmitted Infections – https://www.paho.org/en/topics/sexually-transmitted-infections/syndromic-management-sexually-transmitted-infections
- Advancing STI care in low/middle-income countries: has STI syndromic management reached its use-by date? – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5505769/
- STI Health Disparities: A Systematic Review and Meta-Analysis of the Effectiveness of Preventive Interventions in Educational Settings – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6313766/
- Prevention – https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/stis/prevention
- Advances and challenges in sexually transmitted infections prevention among men who have sex with men in Asia – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9794152/
- Improving care for sexually transmitted infections – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6715945/
- New strategies to tackle and end STIs epidemics – https://www.who.int/news/item/02-09-2022-new-strategies-to-tackle-and-end-stis-epidemics
- Sexually Transmitted Infections – https://www.paho.org/en/topics/sexually-transmitted-infections
- WHO report shows sexually transmitted infections are climbing – https://www.cidrap.umn.edu/sexually-transmitted-infections/who-report-shows-sexually-transmitted-infections-are-climbing
- WORLD HEALTH ORGANIZATION GLOBAL HEALTH SECTOR STRATEGY ON SEXUALLY TRANSMITTED INFECTIONS: AN EVIDENCE-TO-ACTION SUMMARY FOR COLOMBIA – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6754340/
- Sexually Transmitted Infections Surveillance, 2022 – https://www.cdc.gov/std/statistics/2022/default.htm
- STI National Strategic Plan Overview – https://www.hhs.gov/programs/topic-sites/sexually-transmitted-infections/plan-overview/index.html
- Incidence Trends of Five Common Sexually Transmitted Infections Excluding HIV From 1990 to 2019 at the Global, Regional, and National Levels: Results From the Global Burden of Disease Study 2019 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8924524/
- Sexually Transmitted Diseases Among Adolescents in Developed Countries – https://www.guttmacher.org/journals/psrh/2001/01/sexually-transmitted-diseases-among-adolescents-developed-countries
- Sexually transmitted diseases (STDs) in the world – https://academic.oup.com/femspd/article/24/4/431/503360