Your cart is currently empty!
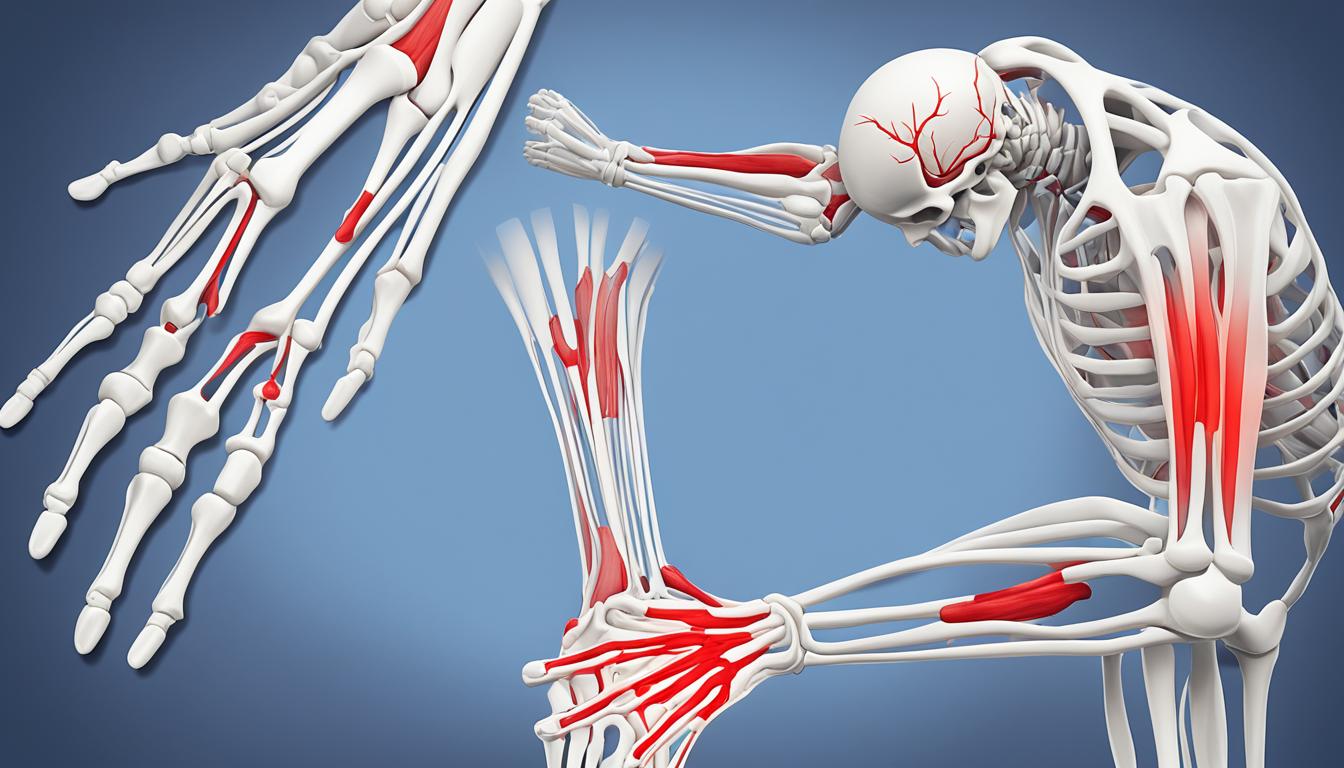
Rheumatoid Arthritis: Causes, Symptoms, and Treatment
Imagine a world where over 50% of early deaths in people with rheumatoid arthritis (RA) are from heart disease. This fact shows how serious RA can be, shortening lives by 3 to 10 years1. But what is this condition, and how can we manage it? We’re going to explore the causes, symptoms, and treatment options for rheumatoid arthritis. This guide aims to give you the knowledge to understand and deal with this complex disease.
Key Takeaways
- Rheumatoid arthritis is an autoimmune disorder that causes joint inflammation and damage to the synovium, the tissue lining the joints.
- Genetic and environmental factors, such as smoking and being overweight, can increase the risk of developing rheumatoid arthritis.
- Early symptoms include joint pain, swelling, and stiffness, which progress through four stages of the disease.
- Diagnosis involves medical history, physical examination, blood tests, and imaging tests like X-rays, ultrasound, and MRI.
- Treatment aims to stop inflammation, relieve symptoms, prevent damage, and improve function, using medications and a treat-to-target approach with tight control.
What is Rheumatoid Arthritis?
Rheumatoid arthritis is an autoimmune disorder that mainly affects the joints2. It happens when the immune system attacks the body’s own cells. This leads to inflammation and damage to the synovium, the tissue around the joints2. The joint capsule gets thicker, causing pain, swelling, and stiffness in the affected joints2.
Rheumatoid Arthritis: An Autoimmune Disorder
Rheumatoid arthritis is an autoimmune disorder. The immune system, meant to fight infections, attacks the body’s healthy tissues instead2. This leads to chronic inflammation. It can cause permanent damage to the joints and other organs2.
Joint Inflammation and Synovium Damage
In rheumatoid arthritis, the synovium lining the joints gets inflamed and thick3. This makes the joint capsule swell, causing pain, stiffness, and less mobility3. Over time, it can also damage the cartilage and bone in the joint, making it harder to move3.
“Rheumatoid arthritis is an autoimmune disorder that causes chronic inflammation of the joints. This can lead to permanent damage and disability if not properly managed.”
Causes of Rheumatoid Arthritis
The exact causes of rheumatoid arthritis are still not fully known. It’s thought to be a mix of genetic and environmental factors that lead to an immune system imbalance4. Some genes might make people more likely to get rheumatoid arthritis. At the same time, things like infections, stress, or other triggers can make the immune system attack the body’s own tissues.
Genetic Factors and Environmental Triggers
Rheumatoid arthritis is an autoimmune disorder, meaning the immune system attacks healthy body tissues by mistake5. Certain genetic changes can increase the risk of getting rheumatoid arthritis. If someone in your family has it, you’re more likely to get it too6. Also, things like infections, chemicals, or toxins, and stress can set off an immune system reaction. This reaction leads to joint inflammation and damage.
Immune System Deregulation
At the heart of rheumatoid arthritis is an immune system imbalance4. In people with rheumatoid arthritis, the immune system’s T cells and B cells see the body’s own tissues as foreign. This leads to ongoing inflammation and joint damage5. This problem can also affect other parts of the body, like the eyes, heart, lungs, and blood vessels.
Understanding how genetic, environmental, and immune factors work together is key to treating rheumatoid arthritis6. By tackling these causes, doctors can help reduce symptoms, stop further joint damage, and improve life for those with this chronic condition.
“Rheumatoid arthritis is a chronic condition that does not disappear. While symptoms may vary and periods of remission may occur, joint damage is irreversible without proper treatment, potentially leading to long-term cartilage and organ harm.”
| Genetic Factors | Environmental Triggers | Immune System Deregulation |
|---|---|---|
| Certain genetic variations can increase the risk of developing rheumatoid arthritis. | Infections, exposure to chemicals/toxins, and psychological stress may trigger the immune system’s abnormal response. | In rheumatoid arthritis, the immune system’s T cells and B cells mistakenly attack the body’s own joint tissues. |
| Having a family member with rheumatoid arthritis raises the odds of developing the condition. | Environmental factors can activate the immune system, leading to chronic inflammation and joint damage. | Immune system dysfunction can also cause problems in other parts of the body, such as the eyes, heart, lungs, and blood vessels. |
Symptoms of Rheumatoid Arthritis
Rheumatoid arthritis brings many symptoms that can really change a person’s life1. Early on, it shows up with tenderness, pain, swelling, and stiffness in joints, like those in the hands and feet1. These symptoms can come and go, lasting over six weeks1. As it gets worse, the inflammation can damage joints and limit how much you can move.
Early Signs of Rheumatoid Arthritis
In the early days, rheumatoid arthritis can be hard to tell apart from other joint issues7. It usually hits smaller joints, like those in the hands, wrists, and feet7. The first signs are often joint pain, swelling, and stiffness1. Some people might also feel tired, have a fever, or lose weight1.
Joint Pain, Swelling, and Stiffness
Joint pain, swelling, and stiffness are key signs of rheumatoid arthritis1. These issues are usually worse in the morning and get better as the day goes on1. The inflammation makes moving hard and can make everyday tasks tough1. Catching it early and treating it is key to easing these symptoms and stopping more damage1.
| Symptom | Description |
|---|---|
| Joint Pain | The affected joints may feel tender, sore, and painful, especially with movement. |
| Joint Swelling | The joints may appear visibly swollen, warm to the touch, and feel inflamed. |
| Joint Stiffness | Individuals may experience difficulty moving or bending the affected joints, particularly in the morning. |
“Rheumatoid arthritis can cause a wide range of symptoms, from joint pain and swelling to fatigue and fever. Early recognition and treatment are crucial in managing this chronic condition.”
Rheumatoid arthritis can really affect someone’s life, so seeing a doctor quickly is key if you notice these signs1. With the right treatment and care, people with rheumatoid arthritis can feel better and stay active and independent187.
Stages of Rheumatoid Arthritis
Rheumatoid arthritis is a condition that gets worse over time and has four main stages. Knowing about these stages helps with early diagnosis and managing the disease. It also helps keep joints healthy over time.
In the initial stage, the joints get inflamed but don’t show any damage yet. This stage brings stiffness, mainly in the smaller joints like those in the hands and feet9. It’s important to see a doctor early here because early treatment can make a big difference.
The second stage sees the cartilage start to break down. Inflammation gets worse, causing swelling and less movement in the joints9. Even before symptoms show, antibodies might be there.
The third stage brings severe inflammation that harms the bones. The joint space gets smaller, and bones may start to wear away9. This stage can cause visible changes in the joints, more pain, and disability.
In the final, or end-stage, inflammation may stop, but the joints keep getting worse10. This can lead to fused joints, less mobility, and a big impact on life quality11. Surgery like joint replacement or fusion might be needed to help with function and pain.
It’s key to start treatment early and aggressively to slow down rheumatoid arthritis10. With a rheumatologist’s help and a good treatment plan, many people with RA can stop the disease from getting worse. This reduces the chance of permanent damage and disability.

Diagnostic Tests for Rheumatoid Arthritis
Diagnosing rheumatoid arthritis requires a detailed look at the patient’s medical history and physical condition12. Doctors start by reviewing the patient’s symptoms and family health history13. Then, they check the affected joints for signs of swelling and pain.
Medical History and Physical Examination
The medical history and physical check-up are key in spotting rheumatoid arthritis13. Doctors look for certain patterns in joint pain and how long symptoms last13. This helps them understand the condition better.
Blood Tests for Inflammation and Antibodies
Blood tests are vital in diagnosing rheumatoid arthritis12. Tests like the ESR and CRP check for inflammation1214. Tests for RF and anti-CCP antibodies confirm the diagnosis121413.
Imaging Tests: X-rays, Ultrasound, and MRI
Imaging tests like X-rays, ultrasound, and MRI show how much joint damage there is1413. X-rays show joint damage and space narrowing. Ultrasound and MRI spot inflammation and early damage not seen on X-rays14.
Diagnosing rheumatoid arthritis is a detailed process13. It uses medical history, physical checks, and tests121413. These tools help doctors find the condition and plan treatment to ease symptoms and prevent more damage121413.
Treatment Options for Rheumatoid Arthritis
Managing rheumatoid arthritis is key to controlling inflammation, easing symptoms, and stopping damage to joints and organs. Doctors use a strong, early treatment plan. This plan includes medications like DMARDs, biologics, and steroids15.
Medications for Rheumatoid Arthritis
Methotrexate is often the first treatment for rheumatoid arthritis, given with another DMARD and steroids15. Side effects can include feeling sick, losing appetite, a sore mouth, diarrhea, headaches, and hair loss15. Biological treatments like adalimumab, etanercept, and infliximab are added if methotrexate alone doesn’t work well15. JAK inhibitors are new medicines for adults with severe rheumatoid arthritis who can’t use DMARDs or biological treatments15. NSAIDs like ibuprofen help with pain and reduce joint inflammation15. Steroids help with pain, stiffness, and inflammation in the short term, especially during a flare-up15.
Treat-to-Target Approach and Tight Control
The main goal of treating rheumatoid arthritis is to reach remission or low disease activity. Doctors use a “treat-to-target” approach, watching the patient’s condition closely and adjusting treatments as needed1516. This strategy, known as “tight control,” greatly improves outcomes for people with rheumatoid arthritis16.
Other treatments like physiotherapy, surgery, and complementary therapies are also part of managing rheumatoid arthritis1516.
“DMARDs have made major improvements in severe rheumatoid arthritis, helping to save joints.”16
Early, strong treatment with a mix of medications is key to managing rheumatoid arthritis and preventing long-term issues17. The treat-to-target approach and tight control let doctors closely watch the disease and adjust treatments for the best results1516.
Self-Care Strategies for Rheumatoid Arthritis
Living with rheumatoid arthritis (RA) means you need a plan that covers many areas. Self-care is key to handling the condition. By adding healthy habits and trying new therapies, you can boost your health and life quality.
Healthy Diet and Exercise
Eating right is vital for those with RA. About two-thirds of people with RA are overweight or obese, which can make treatments less effective18. Foods like salmon, trout, tuna, and sardines can lessen joint pain and stiffness19. Whole grains, such as oatmeal and brown rice, help keep inflammation down19. Exercise is also important. It keeps joints moving, strengthens muscles, and boosts your mood and health.
Hot and Cold Therapies
Heat and cold can help during RA flare-ups. Cold therapy, like ice packs, is good for sudden pain and20. Heat therapy eases pain and stiffness by improving blood flow and relaxing muscles20. These methods are simple and don’t need medicine, making them great for RA self-care.
Stress Reduction and Complementary Therapies
Stress can make RA worse, so finding ways to reduce it is key. Practices like deep breathing, yoga, and can help manage stress and pain19. Other therapies, like massage and acupuncture, might also help18. Adding these holistic methods to your routine can support your overall health.
Always use self-care along with your doctor’s advice. By taking charge of your RA, you can better manage your symptoms, stay independent, and live a fuller life181920.
Complications of Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a complex autoimmune disorder that affects more than just the joints21. It can lead to problems in the eyes, mouth, skin, lungs, blood vessels, and heart. This shows how widespread the effects of RA can be.
One eye issue is dry eyes, also known as Sjögren’s syndrome. RA can cause inflammation and damage to the tear glands. This leads to chronic eye dryness, pain, and sensitivity to light21. It can also cause inflammation of the sclera and cornea.
In the mouth, RA can lead to gum inflammation and a dry mouth condition called xerostomia21. These issues can make dental problems more likely and eating and swallowing harder.
Skin problems include rheumatoid nodules, which are firm lumps under the skin, often near the joints21. These nodules can be painful and can also appear in other areas, like the lungs.
Lung issues are another concern with RA. It can cause inflammation and scarring of the lung tissue, known as interstitial lung disease22. This can lead to breathing problems, reduced lung function, and an increased risk of infections.
RA can also damage blood vessels. The chronic inflammation can affect nerves, skin, and other organs. This can cause vasculitis and Raynaud’s phenomenon, which is reduced blood flow to the fingers and toes22.
Lastly, RA can affect the heart. Inflammation can harm the heart muscle and surrounding tissue, raising the risk of heart attacks and strokes22.
People with RA need to know about these possible complications. Working closely with their healthcare team is key. Early treatment and regular check-ups can reduce the risk of these issues and improve outcomes212223.

Living with Rheumatoid Arthritis
Living with rheumatoid arthritis is tough, but you can manage it with the right strategies and support24. It’s important to handle flare-ups and fatigue to keep a good life and stay independent24.
Managing Flare-Ups and Fatigue
Rheumatoid arthritis brings on flare-ups with more pain, swelling, and stiffness25. These flare-ups can really affect your daily life and health. Knowing what triggers them, like stress or too much work, helps you manage them better25. Also, tracking your disease activity score (DAS) helps doctors adjust your treatment to lessen flare-ups24.
Fatigue is a big issue for people with rheumatoid arthritis25. Feeling tired all the time makes simple tasks hard. To fight fatigue, try pacing yourself, taking breaks, and doing exercises that are easy on your joints24.
Building a Support System
Dealing with rheumatoid arthritis’s physical and emotional sides is tough, but having a strong support system helps a lot. Connecting with family, friends, and groups gives you a sense of belonging, understanding, and help25. Groups like Versus Arthritis and the National Rheumatoid Arthritis Society offer great resources on exercise, pain control, and managing your condition24.
It’s also key to look after your mental health. Depression, stress, and anxiety can come from living with the disease’s physical limits and uncertainty24. Talking to mental health experts or joining groups can help you cope and stay positive25.
If you’re thinking about having a family, talk to your healthcare team about how rheumatoid arthritis and your meds might affect that24. Also, dealing with how rheumatoid arthritis affects your love life and relationships can make you feel better, and there are resources to help with these issues25.
Handling rheumatoid arthritis means using a mix of good medicine, making lifestyle changes, and having strong support. By managing flare-ups, fighting fatigue, and building a support network, you can adapt and live well with this condition24.
Rheumatoid Arthritis and Disability
Rheumatoid arthritis (RA) is more than just a painful joint condition. It can greatly affect daily activities, making people eligible for disability under the Americans with Disabilities Act (ADA)26.
A study showed that 35% of people with RA stopped working within 10 years after their first diagnosis26. This highlights how RA can be very challenging and affect employment. The ADA offers legal support and accommodations for those with RA who are disabled.
To get disability benefits, people with RA must show that their condition limits major life activities like walking, standing, or taking care of themselves. Medical News Today and The Arthritis Foundation offer guidance on how to qualify for RA disability.
The Social Security Administration (SSA) decides if someone is disabled27. Those who qualify might get Social Security Disability Insurance (SSDI) or Supplemental Security Income (SSI) benefits. These benefits can help with financial needs27.
| Disability Benefit | Eligibility Criteria | Average Monthly Benefit |
|---|---|---|
| SSDI | $1,310 for those under 6526 | |
| SSI | Limited income and assets | Varies based on individual circumstances |
Getting through the disability claims process can be tough, but there’s help for people with RA. Healthline offers steps to qualify for disability benefits and ADA legal protections.
“Rheumatoid arthritis can be a debilitating condition, but the ADA and disability benefits can provide crucial support for those who qualify. It’s important for individuals with RA to understand their rights and explore all available options.”
Understanding how RA affects disability helps people take steps to protect their financial and personal well-being. With the right support and accommodations, those with RA can still lead fulfilling lives despite the challenges.
Rheumatoid Arthritis: Key Differences
Rheumatoid arthritis (RA) and osteoarthritis (OA) are both types of arthritis. But they have different causes and signs28. RA is an autoimmune disease where the body attacks the joints by mistake, causing inflammation and damage28. OA, on the other hand, happens when cartilage breaks down over time.
Rheumatoid Arthritis vs. Osteoarthritis
RA and OA both cause joint pain and stiffness, but they are not the same28. RA usually affects the small joints in the hands and feet, while OA often hits the hips and knees28. RA also brings morning stiffness that lasts an hour or more, which OA doesn’t usually do28.
RA affects more than just the joints; it can impact the whole body, leading to fatigue, low fevers, and rheumatoid nodules2829. It’s also much rarer than OA, affecting only 1% of people in the UK, compared to OA which affects one-third of those over 4529.
Rheumatoid Arthritis vs. Gout
Gout and RA are both painful arthritis types, but they have different causes28. Gout comes from uric acid crystals building up in the joints, often in the big toe. RA is caused by an immune system that attacks the joints28.
Gout usually hits one joint, while RA affects multiple joints at once, especially the small ones in the hands and feet28.
Handling RA and gout also varies28. RA is treated by specialists, while OA is often handled by general doctors28. RA treatment uses drugs like DMARDs to control the immune system and stop the disease from getting worse28. Gout treatment focuses on lowering uric acid levels and controlling flare-ups292830.
Conclusion
Rheumatoid arthritis is a complex autoimmune disorder that can greatly affect someone’s life31. But, with early diagnosis and the right treatment, many people can control their symptoms and live fully31. In the U.S., about 0.6% of people have this condition, and women are more likely to get it than men31.
In the past 20 years, how we treat rheumatoid arthritis has changed a lot. Now, patients get better care, which has lowered the disease’s activity levels32. Both traditional and biological treatments work well, and new criteria help diagnose it earlier31. The main aim of treatment is to stop inflammation and prevent long-term damage31.
Even though rheumatoid arthritis is ongoing, the right care and a positive attitude can help manage it31. By staying informed and having a strong support system, people with this condition can overcome its challenges. They can focus on what’s important to them.
FAQ
What is rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune disorder. It causes joint inflammation and damage to the synovium. This is the tissue lining the joints.
What are the causes of rheumatoid arthritis?
It’s thought to be caused by a mix of genetic and environmental factors. These lead to an immune system imbalance.
What are the early symptoms of rheumatoid arthritis?
Early signs include tenderness, pain, swelling, and stiffness in joints. This is often in the smaller joints of the hands and feet.
How does rheumatoid arthritis progress?
It goes through four main stages. From inflammation in the joint tissue to severe pain, swelling, stiffness, and loss of mobility.
How is rheumatoid arthritis diagnosed?
Diagnosis includes a detailed medical history, physical check-up, blood tests for inflammation and autoantibodies, and imaging tests like X-rays, ultrasound, and MRI.
What are the treatment options for rheumatoid arthritis?
Treatment focuses on stopping inflammation, easing symptoms, preventing damage, and improving function. It uses medications and a treat-to-target approach with tight control.
What self-care strategies can help manage rheumatoid arthritis?
Eating a balanced diet and staying active are key. Using hot and cold therapies, reducing stress, and trying complementary therapies also help manage symptoms.
What are the potential complications of rheumatoid arthritis?
It can cause complications in the eyes, mouth, skin, lungs, blood vessels, and heart.
How can individuals cope with living with rheumatoid arthritis?
Managing flare-ups and fatigue is important. Building a strong support system with family, friends, and healthcare providers helps with the physical and emotional challenges.
Can rheumatoid arthritis qualify as a disability?
If it limits one or more major life activities, the person may get disability benefits under the Americans with Disabilities Act (ADA).
How does rheumatoid arthritis differ from other types of arthritis?
It’s an autoimmune disorder. Unlike osteoarthritis, which is from cartilage wear, and gout from uric acid crystals buildup.
Source Links
- Everything You Want to Know About Rheumatoid Arthritis – https://www.healthline.com/health/rheumatoid-arthritis
- Rheumatoid Arthritis – https://www.cdc.gov/arthritis/rheumatoid-arthritis/index.html
- Rheumatoid arthritis – https://www.nhs.uk/conditions/rheumatoid-arthritis/
- Rheumatoid Arthritis (RA): Causes, Symptoms & Treatment FAQs – https://my.clevelandclinic.org/health/diseases/4924-rheumatoid-arthritis
- No title found – https://www.arthritis.org/diseases/rheumatoid-arthritis
- Rheumatoid Arthritis – https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
- What Are Rheumatoid Arthritis Symptoms? – https://www.massgeneralbrigham.org/en/about/newsroom/articles/symptoms-of-rheumatoid-arthritis
- Rheumatoid Arthritis (RA): Practice Essentials, Background, Pathophysiology – https://emedicine.medscape.com/article/331715-overview
- The 4 Stages of Rheumatoid Arthritis Progression – https://creakyjoints.org/about-arthritis/rheumatoid-arthritis/ra-overview/rheumatoid-arthritis-stages-progression/
- Progression of Rheumatoid Arthritis – https://www.webmd.com/rheumatoid-arthritis/ra-progression
- Rheumatoid Arthritis Stages: 1 to 4, Progression, and More – https://www.healthline.com/health/rheumatoid-arthritis/stages-and-progression
- Rheumatoid arthritis – Diagnosis and treatment – Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/drc-20353653
- Rheumatoid Arthritis – https://www.niams.nih.gov/health-topics/rheumatoid-arthritis/diagnosis-treatment-and-steps-to-take
- Rheumatoid arthritis – Diagnosis – https://www.nhs.uk/conditions/rheumatoid-arthritis/diagnosis/
- Rheumatoid arthritis – Treatment – https://www.nhs.uk/conditions/rheumatoid-arthritis/treatment/
- Understanding Rheumatoid Arthritis: Treatment – https://www.webmd.com/rheumatoid-arthritis/understanding-rheumatoid-arthritis-treatment
- Approach Considerations, Pharmacologic Therapy, Considerations for Specific Patient Presentations – https://emedicine.medscape.com/article/331715-treatment
- Self-Help and Living with Rheumatoid Arthritis – https://www.news-medical.net/health/Self-Help-and-Living-with-Rheumatoid-Arthritis.aspx
- How to Take Care of Your Rheumatoid Arthritis. Tips for a Better Life – https://www.webmd.com/rheumatoid-arthritis/tips-living-with-ra
- Tips to Ease RA Flare – https://www.webmd.com/rheumatoid-arthritis/self-care-rheumatoid-arthritis
- Rheumatoid Arthritis (RA) Symptoms and Complications – https://www.webmd.com/rheumatoid-arthritis/rheumatoid-arthritis-symptoms
- Rheumatoid arthritis – Complications – https://www.nhs.uk/conditions/rheumatoid-arthritis/complications/
- Systemic complications of rheumatoid arthritis: Focus on pathogenesis and treatment – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9817137/
- Rheumatoid arthritis – Living with – https://www.nhs.uk/conditions/rheumatoid-arthritis/living-with/
- Rheumatoid arthritis: Learn More – Everyday life with rheumatoid arthritis – InformedHealth.org – https://www.ncbi.nlm.nih.gov/books/NBK384458/
- Is rheumatoid arthritis a disability? Benefits and more – https://www.medicalnewstoday.com/articles/is-rheumatoid-arthritis-a-disability
- No title found – https://www.arthritis.org/health-wellness/healthy-living/daily-living/disability-for-arthritis-how-qualify-for-benefits
- Comparing RA and OA – https://www.webmd.com/rheumatoid-arthritis/rheumatoid-arthritis-osteoarthritis-difference
- Rheumatoid arthritis (RA) and Osteoarthritis (OA) key differences | NRAS – https://nras.org.uk/resource/rheumatoid-arthritis-ra-and-osteoarthritis-oa/
- Rheumatoid arthritis (RA) – https://versusarthritis.org/about-arthritis/conditions/rheumatoid-arthritis/
- Review of Rheumatoid Arthritis – https://www.uspharmacist.com/article/review-of-rheumatoid-arthritis
- Conclusions and recommendations – Intensive therapy for moderate established rheumatoid arthritis: the TITRATE research programme – https://www.ncbi.nlm.nih.gov/books/NBK572919/