Your cart is currently empty!
Ulcerative Colitis: Causes, Symptoms, and Treatment
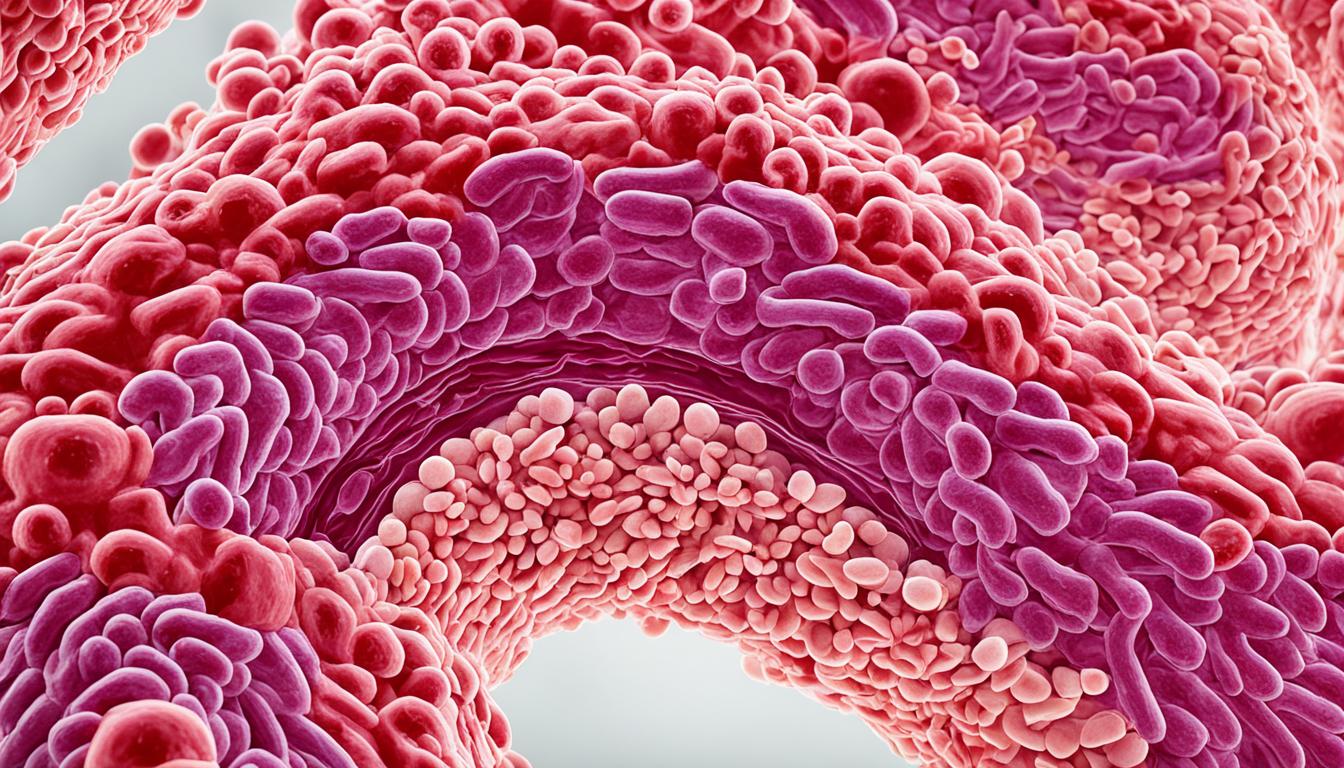
Ulcerative colitis affects nearly 1 million Americans, making it a major health issue1. It’s a chronic condition that causes inflammation and damage in the large intestine. This leads to many uncomfortable symptoms and can cause serious problems. Knowing about its causes, symptoms, and treatments is key to handling this condition.
Key Takeaways
- Ulcerative colitis usually starts in people between 15 and 30 years old1.
- Symptoms include diarrhea, mucus and blood in stool, stomach pain, and losing weight1.
- It’s connected to genetics, infections, and lifestyle factors like diet1.
- Treatments include medicines, surgery, and changing your diet to ease symptoms1.
- Ulcerative colitis raises the risk of getting bowel cancer over time1.
What is Ulcerative Colitis?
Definition and Overview
Ulcerative colitis is a chronic condition that causes inflammation and ulcers in the colon’s lining2. It’s a painful condition that can greatly affect someone’s life. While there’s no cure, treatments help manage symptoms and prevent serious problems2.
About a million Americans have ulcerative colitis, making it the most common inflammatory bowel disease2. Most people get diagnosed before they turn 30, but it can happen at any age2. Whites, especially those of Ashkenazi Jewish descent, and people with a family history are more likely to get it2.
Symptoms include diarrhea with blood or pus, fever, and feeling very tired2. Other symptoms are anemia, abdominal pain, rectal pain, bleeding, and losing weight2. Over time, it can lead to dehydration, bone loss, and a higher risk of colon cancer2.
The only sure way to diagnose it is through a biopsy during an endoscopy2. Other tests may be done first to check for other conditions2. Treatment options include drugs, surgery to remove damaged tissue, and sometimes removing the whole colon2.
“Ulcerative colitis is a chronic, inflammatory bowel disease that affects the colon and rectum, causing inflammation, ulcers, and other complications that can significantly impact a person’s quality of life.”
Who is at Risk for Ulcerative Colitis?
Ulcerative colitis is a complex condition, and its exact cause is still unknown. Yet, some factors can raise a person’s risk of getting this inflammatory bowel disease3.
Age is a big risk factor, with most diagnoses happening before age 30 or after age 604. People of Caucasian and Ashkenazi Jewish descent face a higher risk than those of African or Asian ancestry3.
Having a family history is also a key risk factor. If a close relative has ulcerative colitis, your risk goes up by up to 30%4. Research shows that the risk can range from 1.6 percent to 30 percent if you have a first-degree relative with the disease4.
Diet and stress don’t directly cause ulcerative colitis but can make symptoms worse3. Eating too much sugar and fat, not enough fiber, and stress can up your risk3.
Some studies suggest that removing the appendix before age 20 might lower ulcerative colitis risk3. But, using broad-spectrum antibiotics could increase your risk3.
Even though we don’t know the exact cause of ulcerative colitis, knowing the risk factors helps. It helps both individuals and doctors spot those at higher risk and manage the condition better345.
“Ulcerative colitis is a complex condition, and the exact cause remains unknown. However, certain demographic and lifestyle factors can increase an individual’s risk of developing this inflammatory bowel disease.”
Symptoms of Ulcerative Colitis
Ulcerative colitis is a chronic disease that affects the large intestine’s lining. It causes many distressing symptoms6. One key sign is bloody diarrhea, which might also have pus7. People with this condition often feel the need to have a bowel movement suddenly, leading to cramps and a loss of appetite.
This can result in weight loss and feeling very tired7. In severe cases, someone might have more than 10 bloody bowel movements a day8. Other symptoms include fever, nausea, vomiting, and pain in the joints, especially if the disease affects more of the large intestine7.
The symptoms of ulcerative colitis can change over time, with periods of remission and flare-ups7. Researchers think genetics, immune system issues, and environmental factors contribute to the disease76. It’s more common in certain groups like Europeans and Ashkenazi Jews, but it can happen to anyone6.
Getting an accurate diagnosis is key to managing ulcerative colitis8. Doctors use blood tests, scans, flexible sigmoidoscopy, and colonoscopy to check the condition and track its progress8.
“Understanding the symptoms of ulcerative colitis is the first step towards effective management and improving quality of life for those living with this chronic condition.”
Types of Ulcerative Colitis
Ulcerative colitis is a complex condition with different forms, each with unique characteristics. The types of ulcerative colitis are based on where and how much the colon gets inflamed.9
Proctitis, Proctosigmoiditis, Left-sided Colitis, and Pancolitis
Proctitis is one of the milder forms, affecting only the rectum9. People with this type often feel pain, bleed, and need to go to the bathroom urgently9.
Proctosigmoiditis affects the rectum and the lower part of the colon, the sigmoid colon. Symptoms include losing appetite, losing weight, pain on the left side of the abdomen, and bloody stools9.
Left-sided colitis starts at the rectum and moves up the left side of the colon. Those with this type may have bloody stools, pain, losing weight, not wanting to eat, fever, and cramps9.
The most severe form is pancolitis, affecting the whole colon. It brings the worst symptoms, like bloody stools, pain, losing weight, not eating well, fever, and cramps9.
Knowing the type of ulcerative colitis helps in choosing the right treatment and managing the condition9.
“The location and extent of inflammation in the colon can have a significant impact on the symptoms and management of ulcerative colitis.”
Diagnosing Ulcerative Colitis
Doctors use a mix of medical history, physical checks, and tests to diagnose ulcerative colitis. They start by looking at the patient’s past health and family history for signs and risk factors10.
The doctor will then perform a physical exam to check vital signs and listen to the abdomen10. Blood tests are done to find signs of ulcerative colitis, like anemia or infections10. They might also take stool samples to check for infections and inflammation10.
To be sure of the diagnosis, a colonoscopy or flexible sigmoidoscopy is usually needed10. These tests let the doctor see the colon and take tissue samples for tests10. Imaging tests like x-rays or CT scans can also show how much the colon is inflamed10.
Doctors also look at lifestyle habits, like smoking, which can affect ulcerative colitis10.
Getting the diagnosis right is key to treating ulcerative colitis well. By using medical history, physical exams, and tests, doctors can confirm the diagnosis and see how bad it is10.
Blood tests, stool studies, endoscopic procedures, and imaging tests are key in diagnosing ulcerative colitis11. These tests help spot inflammation, rule out other conditions, and help decide on treatment11. Doctors might prescribe medicines or surgery for severe cases11. They also suggest regular cancer screenings because of the higher risk of colorectal cancer11.
Blood tests can find signs of infection and anemia, which might mean bleeding in the colon or rectum12. X-rays with contrast can show the GI tract in detail12. Endoscopies let doctors directly examine the colon and rectum, and chromoendoscopy helps find polyps or early cancer signs12. Biopsies from endoscopies are vital for further testing12.
Getting ulcerative colitis diagnosed right is crucial for a good treatment plan. By using a thorough approach with medical history, physical exams, and various tests, doctors can give the best care to patients with ulcerative colitis101112.
Treatment Options for Ulcerative Colitis
Medications, Surgery, and Diet
There is no cure for ulcerative colitis, but many treatments can help manage symptoms and achieve remission13. These include medications, surgery, and changing your diet.
Medications for Ulcerative Colitis
Doctors use anti-inflammatory drugs, immune system suppressants, biologics, and other therapies to treat ulcerative colitis14. For mild to moderate cases, aminosalicylates, or 5-ASAs, are often the first choice14. Corticosteroids like prednisolone help during flare-ups, while immunosuppressants keep the disease in remission14. Biologics are used for more severe cases and come as infusions or injections15.
Surgery for Ulcerative Colitis
Surgery might be needed if other treatments don’t work or if complications happen13. This usually means removing the colon (colectomy) or the colon and rectum (proctocolectomy)15. Surgery is considered when the disease greatly affects a person’s life or there are concerns about future problems14.
Dietary Changes for Ulcerative Colitis
Changing what you eat can also help manage ulcerative colitis13. People with this condition often avoid foods like dairy, caffeine, alcohol, and high-fiber items that can make symptoms worse13. Eating a balanced diet with soft, easy-to-digest foods is recommended13.
By using these treatments together, doctors can help people with ulcerative colitis get and stay in remission, improving their life quality13. Researchers are always looking for new and better treatments for this chronic condition13.

“Maintaining good nutrition is crucial for individuals with ulcerative colitis as the disease often reduces appetite while increasing the body’s energy needs.”
| Treatment Approach | Description |
|---|---|
| Medications |
|
| Surgery |
|
| Dietary Changes |
|
Complications of Ulcerative Colitis
Ulcerative colitis is a chronic disease that can cause serious problems if not treated16. About 1 in 3 people with this condition also get inflammation in other parts of their body16. These issues can greatly affect someone’s life and health. It’s crucial to see a doctor quickly and follow a treatment plan.
Bleeding is a possible complication of ulcerative colitis17. Sometimes, bleeding can start weeks or months before symptoms appear17. The severity of symptoms can vary a lot, from mild to severe17. This bleeding can lead to anemia, causing tiredness, weakness, and other health problems16. Dehydration is also common due to the diarrhea that comes with the disease.
16 People with ulcerative colitis might also get osteoporosis because of medication side effects and changes in diet16. Kids and young adults may not grow well and may not reach puberty on time, showing why early diagnosis and good management are key.
Severe cases of ulcerative colitis can lead to16 toxic megacolon, a rare but serious condition that can cause the colon to rupture18. Symptoms include severe stomach pain, high fever, and a fast heart rate18. Those with ulcerative colitis are also at higher risk of getting primary sclerosing cholangitis and bowel cancer, especially if the disease is severe or affects most of the colon.
Quick treatment and regular check-ups are vital to avoid or manage ulcerative colitis complications18. For some, this condition can be very serious and even life-threatening. That’s why it’s important to work closely with doctors to manage it well.
| Complication | Description | Prevalence |
|---|---|---|
| Extra-intestinal manifestations | Inflammation in other parts of the body | Around 1 in 3 people with ulcerative colitis |
| Osteoporosis | Decreased bone density due to medications and dietary changes | Increased risk in people with ulcerative colitis |
| Poor growth and delayed puberty | Seen in children and young people with ulcerative colitis | Not specified |
| Toxic megacolon | Rare condition that can result in colon rupture | Not specified |
| Primary sclerosing cholangitis | Condition affecting the bile ducts | Increased risk in people with ulcerative colitis |
| Colon cancer | Elevated risk, especially with severe or widespread disease | Increased risk in people with ulcerative colitis |
Living with Ulcerative Colitis
Living with ulcerative colitis can be tough, but many people manage it well19. It affects about 2.2 to 14.3 people per 100,000, and its cases have been rising over the past 50 years19. Most people get diagnosed in their mid-30s, but it can happen at any age19.
To manage ulcerative colitis, find and avoid your personal triggers, eat well, manage stress, and stick to your treatment plan20. Stress management is key, and you can try joining a support group, exercising, doing yoga or meditation, and learning new ways to handle stress20.
Getting support from doctors, family, and other patients is crucial for dealing with the disease’s effects20. Talking openly about your condition with those close to you can help you manage it better20.
| Key Considerations for Living with Ulcerative Colitis |
|---|
| Identifying and avoiding personal triggers |
| Maintaining a balanced, nutritious diet |
| Practicing stress management techniques |
| Staying consistent with prescribed medications |
| Seeking support from healthcare providers, family, and patient communities |
Ulcerative colitis is a chronic and unpredictable condition, but with the right approach, many people live fulfilling lives19. Research shows that most UC patients live happy and productive lives19.
“Communication with healthcare providers and partners is key in addressing the challenges of living with ulcerative colitis.” – Dr. Jane Doe, Gastroenterologist
Ulcerative Colitis and Pregnancy
Managing ulcerative colitis (UC) during pregnancy can be tough, but many women with UC have successful pregnancies and healthy babies21. Women with inflammatory bowel disease (IBD), like UC, face a higher risk of pregnancy and delivery issues21. Yet, their fertility rates are similar to others, between 5–14%21.
A big study in Europe showed that 67% of people with active UC during pregnancy got better21. If both parents have UC, the chance of the child getting it goes up to 40%. If only one parent has it, the risk is about 9%21.
Most IBD medicines are safe during pregnancy21. But, women with UC should keep taking their medicines as their doctor says, even when pregnant or trying to conceive. Pregnancy doesn’t cure UC and might make symptoms worse, raising the risk of flare-ups2122.
Pregnancy can affect women with IBD, like UC, in different ways23. The risk of pregnancy issues for women with IBD is between 830-837 per 10,00023. Those with Crohn’s disease face a higher risk of giving birth too early23. Women with ulcerative colitis see rates of about 735-742 per 10,00023.
Working together, gastroenterologists and obstetricians are key to giving the best care for mom and baby. With the right team support, women with UC can face pregnancy’s challenges and aim for a healthy pregnancy and baby.
Ulcerative Colitis in Children
Ulcerative colitis is a chronic condition that affects the colon in kids and teens24. Kids with this condition often have diarrhea, stomach pain, and may not grow as they should25. Doctors need to pay special attention to their nutrition, growth, and emotional well-being.
This condition only affects the colon and can cover the whole colon, known as universal colitis25. Kids with it may feel a lot of stomach pain, have diarrhea with blood, feel tired, lose weight, and have a fever25.
The exact cause of ulcerative colitis in kids is still a mystery, but it might be related to an overactive immune system, genes, or reactions to harmless bacteria or things in the environment25. It’s not passed down through genes, but it can run in families, affecting many relatives with different types of bowel diseases25.
At Hassenfeld Children’s Hospital at NYU Langone, experts in Pediatric Gastroenterology diagnose ulcerative colitis in kids26. They use tests like blood work, stool tests, and exams to figure it out26.
- Blood tests can show high white blood cells, platelets, and signs of anemia, and liver tests may show inflammation26.
- Stool tests can find blood and signs of infections like salmonella26.
- Magnetic resonance enterography shows detailed images of the small intestine26.
- Upper endoscopy lets doctors check the lining of the esophagus, stomach, and small intestine26.
- Colonoscopy shows the lining of the colon and rectum for inflammation and ulcers26.
- During colonoscopy, biopsies help tell the difference between ulcerative colitis and Crohn’s disease26.
- Capsule endoscopy uses a camera pill to take pictures of the small intestine26.
Treatment for kids with ulcerative colitis aims to ease symptoms, prevent flare-ups, heal the lining of the colon, and bring on remission24. Doctors use medicines like 5-aminosalicylates, steroids, antibiotics, and more to help24. Sometimes, surgery is needed to improve a child’s life if medicines don’t work well enough24.
In short, ulcerative colitis can happen in kids and teens, causing stomach issues and other problems. Kids need special care, including tests, medicines, and sometimes surgery, to manage this condition.
Ulcerative Colitis Research and Advancements
Ulcerative colitis research is moving fast, with big steps forward in understanding the condition and finding new treatments27. Scientists are looking into the immune system, genes, and the environment to help treat it better28.
Ongoing Studies and Developments
Researchers are looking at many things, like the gut’s bacteria, genes, and new ways to treat it28. A 2020 study showed that some people with ulcerative colitis get pouchitis after surgery, which is ongoing inflammation27. They found that those with pouchitis have fewer certain bacteria and bile acids, which might affect the disease.
The FDA approved vedolizumab (Entyvio) for severe ulcerative colitis in 202027. It’s the only approved treatment for this condition, given by injection or IV27. A study in 2020 showed it’s safe and works well for keeping symptoms under control27.
Other treatments like JAK inhibitors and stem cell transplant are being looked at too27. Scientists are also working on new ways to check inflammation, like wearable devices and pills27.
Research has also found genetic links to ulcerative colitis28. The IBD Genetics Consortium found over 200 genes linked to inflammatory bowel disease, including ulcerative colitis28. The PROTECT study found genes and traits that help predict treatment success in kids with ulcerative colitis28.
These studies and new treatments offer hope for better managing ulcerative colitis and improving life for those with it29.
The hard work of researchers in understanding and treating ulcerative colitis shows their commitment to helping those affected29.
Ulcerative Colitis and Mental Health
Living with ulcerative colitis (UC) can really affect your mental health. People with UC often feel more anxious and depressed than those without it303132. The physical symptoms and limits from UC can be very hard on the mind and emotions, making stress a common trigger for flare-ups3032.
Studies show that mood issues, like depression, can make UC flare-ups come back more often for some30. There might also be a link between inflammation, stress, and mood problems like depression and anxiety in UC patients30. Stress can change gut bacteria, affecting emotions, the immune system, and pain, making the emotional effects worse30.
To help with the mental health side of UC, doctors suggest a full approach. This includes counseling, support groups, and stress-reducing methods like mindfulness-based meditation30. Cognitive behavioral therapy (CBT), gut-directed hypnotherapy, and stress management can also help manage the emotional side of UC3032.
Also, exercise can make UC patients feel better, offering mood benefits similar to antidepressants in some cases30. Talking about antidepressants with a doctor can also help improve mood and ease gut symptoms30. Insomnia, linked to more inflammation and depression in UC patients, can be helped with various treatments30.
Being in nature and spending time outside can also lower anxiety and stress in UC patients30. It’s important to talk openly with doctors about emotional issues related to UC, even if they’re not a mental illness30.

By tackling the emotional side of ulcerative colitis with a wide approach, patients can live better and manage the challenges of this chronic condition303132.
Ulcerative Colitis Diet and Nutrition
An ulcerative colitis diet doesn’t cause the condition, but it can help manage symptoms and improve health33. People with this condition should avoid foods that can make symptoms worse, like dairy, high-fiber foods, spicy foods, and fizzy drinks33. Instead, eating lean proteins, fruits, and vegetables is recommended to help control symptoms.
Good nutrition is key for those with ulcerative colitis33. Studies show that what we eat affects how the condition develops and how well it is managed33. Eating poorly can make symptoms worse and affect health outcomes33.
Some food additives and artificial sweeteners might cause inflammation, making a diet based on whole foods important33. Eating certain foods too often can also lead to inflammation33. A dietitian can help create a meal plan that meets your needs and ensures you get all the nutrients you need, even when you’re sick or in remission.
Nutrition Considerations for Ulcerative Colitis
When you’re having a flare-up, you might need more protein to help your body heal33. It’s important to drink plenty of water, eat nutrient-rich foods, and increase your protein intake33. But, it’s also important not to cut out too many foods to avoid not getting enough nutrients33.
When you’re in remission, you might need to adjust the texture of foods with fiber33. Eating a variety of fruits, vegetables, nuts, seeds, herbs, and whole grains is good for your gut health33. This helps you get all the nutrients you need and supports your overall health.
| Nutrient | Importance for Ulcerative Colitis | Common Deficiencies |
|---|---|---|
| Protein | Increased needs during flares to support healing | Protein losses from inflammation, diarrhea, and malabsorption |
| Calcium and Vitamin D | Essential for bone health, which can be impacted by medications and malabsorption | Many adults, including those with UC, do not consume enough |
| Folate and Vitamin B12 | Required for red blood cell production and DNA synthesis | Malabsorption from medications like sulfasalazine |
| Iron | Needed to prevent anemia, which is common in UC | Blood loss from inflammation and diarrhea |
Keeping a balanced and nutrient-rich diet is crucial for people with ulcerative colitis. Working with healthcare professionals can help create a personalized nutrition plan. This plan can help manage symptoms, prevent complications, and support overall well-being333435.
“Proper nutrition is crucial for individuals living with ulcerative colitis. A balanced, whole-food-based diet can make a significant difference in managing symptoms and supporting overall health.”
Ulcerative Colitis Medications
Types, Side Effects, and Considerations
Managing ulcerative colitis often means picking the right medications for each person. These can be put into different groups, each with its own way of working, benefits, and side effects.
Aminosalicylates like balsalazide, mesalamine, olsalazine, and sulfasalazine are often the first choice for mild to moderate flare-ups. They help reduce inflammation and are effective for many people3637.
Corticosteroids are used for more severe cases of ulcerative colitis. They help lessen inflammation but can have side effects like weight gain, high blood pressure, and a higher chance of infections3637.
If aminosalicylates or corticosteroids don’t work well, doctors might suggest immunomodulators. These include azathioprine, 6-mercaptopurine, cyclosporine, and tacrolimus. They calm down an overactive immune system that can cause ulcerative colitis37.
Recently, a new type of drug called targeted synthetic small molecules has been approved for severe cases. These drugs target specific parts of the inflammatory process, offering a more precise treatment3637.
Biologic therapies are also available for those with moderate to severe ulcerative colitis. They include adalimumab, certolizumab pegol, golimumab, infliximab, ustekinumab, and vedolizumab. These medications focus on certain proteins or cells in the immune system3637.
Even though these medications work well, they can have side effects like liver damage, skin cancers, lymphoma, infections, kidney issues, gout, and high blood pressure38. It’s important to be closely monitored by doctors when taking these drugs.
Choosing and adjusting ulcerative colitis medications is a team effort between the patient and their healthcare team. Things like how severe the disease is, how well previous treatments worked, and how well the body can handle the medication will help decide the best treatment plan.
Conclusion
Ulcerative colitis is a complex condition that affects both the body and mind39. While finding a cure is not possible, new research and treatments help many people manage their symptoms39. Working together with doctors and making progress in science is key to tackling this disease.
The number of people with inflammatory bowel disease, like ulcerative colitis, is going up worldwide4041. Researchers are getting closer to understanding what causes it, looking at genes and environment4041. There are now more ways to treat it, helping patients control symptoms and lower the risk of serious problems like cancer41.
As doctors keep finding new ways to treat ulcerative colitis, it’s important for patients to stay connected with their healthcare team394041. By keeping up with the latest research and working with their doctors, people with ulcerative colitis can better manage their condition. This helps improve their life quality394041.
FAQ
What is ulcerative colitis?
Ulcerative colitis is a chronic condition that causes inflammation and ulcers in the colon’s lining. It’s a type of inflammatory bowel disease.
What are the symptoms of ulcerative colitis?
Symptoms include diarrhea, often with blood or pus, and abdominal pain. People may also feel tired and lose weight.
What causes ulcerative colitis?
The exact cause is still unknown. It might be related to an abnormal immune response or genetics.
Who is at risk for developing ulcerative colitis?
Those at higher risk include certain ages, ethnicities, and those with a family history of the disease.
What are the different types of ulcerative colitis?
There are several types, like proctitis and pancolitis. Each type affects different parts of the colon.
How is ulcerative colitis diagnosed?
Doctors use endoscopies, biopsies, blood tests, and imaging to diagnose it.
What are the treatment options for ulcerative colitis?
Treatments include medications, surgery, and changes to diet.
What are the potential complications of ulcerative colitis?
Complications include bleeding, anemia, dehydration, and a higher risk of colon cancer.
How can people with ulcerative colitis manage their condition?
Managing it means identifying triggers, eating well, managing stress, and sticking to medication.
How does ulcerative colitis affect pregnancy and children?
It can be challenging for pregnant women and children. They need special care and attention.
What advancements are being made in ulcerative colitis research?
Researchers are finding new causes and treatments, like biologics and JAK inhibitors.
How does ulcerative colitis impact mental health?
It can affect mental health by causing anxiety, depression, and stress due to symptoms and limitations.
What role does diet play in managing ulcerative colitis?
Diet doesn’t cause the disease but can help manage symptoms. Working with a dietitian is helpful.
What types of medications are used to treat ulcerative colitis?
Medications include anti-inflammatory drugs, immunosuppressants, biologics, and targeted therapies. Each has its own effects and side effects.
Source Links
- Ulcerative colitis – https://www.healthdirect.gov.au/ulcerative-colitis
- Ulcerative colitis – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-causes/syc-20353326
- Who’s At Risk for Ulcerative Colitis? – https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/uc-who-is-at-risk
- Overview of Ulcerative Colitis – https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ulcerative-colitis/overview
- Ulcerative Colitis – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK459282/
- Ulcerative colitis – https://www.nhs.uk/conditions/ulcerative-colitis/
- Symptoms & Causes of Ulcerative Colitis – NIDDK – https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis/symptoms-causes
- Ulcerative Colitis – https://www.hopkinsmedicine.org/health/conditions-and-diseases/ulcerative-colitis
- Types of Ulcerative Colitis – https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/ulcerative-colitis-types
- Diagnosis of Ulcerative Colitis – NIDDK – https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis/diagnosis
- Ulcerative colitis – Diagnosis and treatment – Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/diagnosis-treatment/drc-20353331
- Ulcerative Colitis Diagnosis and Testing – https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ulcerative-colitis/diagnosis-testing
- Ulcerative Colitis Treatment Options – https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ulcerative-colitis/treatment-options
- Ulcerative colitis – Treatment – https://www.nhs.uk/conditions/ulcerative-colitis/treatment/
- Ulcerative Colitis Treatment Options – https://www.crohnsandcolitis.com/ulcerative-colitis/treatment-options
- Ulcerative colitis – Complications – https://www.nhs.uk/conditions/ulcerative-colitis/complications/
- Clinical manifestations, diagnosis, and prognosis of ulcerative colitis in adults – https://www.uptodate.com/contents/clinical-manifestations-diagnosis-and-prognosis-of-ulcerative-colitis-in-adults
- Inflammatory bowel disease (IBD) – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315
- PDF – https://www.crohnscolitisfoundation.org/sites/default/files/legacy/assets/pdfs/living-with-ulcerative.pdf
- Living With Ulcerative Colitis | Pfizer – https://www.pfizer.com/news/articles/living_with_ulcerative_colitis
- Ulcerative colitis and pregnancy: What is the link? – https://www.medicalnewstoday.com/articles/325184
- Ulcerative Colitis and Pregnancy – https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/uc-pregnancy-faqs
- Pregnancy and Inflammatory Bowel Disease – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4836574/
- Ulcerative Colitis in Children | Children’s Hospital of Philadelphia – https://www.chop.edu/conditions-diseases/ulcerative-colitis-in-children
- ulcerative colitis in children and young people – https://www.cicra.org/what-is-ibd/ulcerative-colitis/
- Diagnosing Ulcerative Colitis in Children – https://www.nyulangone.org/conditions/ulcerative-colitis-in-children/diagnosis
- Ulcerative colitis research update – https://www.medicalnewstoday.com/articles/research-update-ulcerative-colitis
- Clinical Trials for Ulcerative Colitis – NIDDK – https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis/clinical-trials
- Bioengineered approach shows promise in ulcerative colitis – https://www.utsouthwestern.edu/newsroom/articles/year-2024/jan-bioengineered-approach-ulcerative-colitis.html
- Ulcerative Colitis and Your Mental Health: Depression, Anxiety, Stress – https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/ulcerative-colitis-mental-health
- What to know about ulcerative colitis and your mental health – https://www.medicalnewstoday.com/articles/ulcerative-colitis-and-mental-health-link
- Ulcerative Colitis and Your Mental Health – https://health.clevelandclinic.org/taking-care-of-your-mental-health-is-a-key-piece-of-the-ibd-puzzle
- What Should I Eat? – https://www.crohnscolitisfoundation.org/patientsandcaregivers/diet-and-nutrition/what-should-i-eat
- 16178–Nutrition and Ulcerative Colitis (patient handout view) – http://www.healthsystem.virginia.edu/docs/per/nutrition-and-ulcerative-colitis/handout_view_patient/@@getDocument
- Nutrition Tips for Inflammatory Bowel Disease – https://www.ucsfhealth.org/education/nutrition-tips-for-inflammatory-bowel-disease
- Medication Options for Ulcerative Colitis – https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ulcerative-colitis/medication
- Ulcerative Colitis Treatments and Surgery – https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/digestive-diseases-ulcerative-colitis-treatment
- Which Prescription Drugs Treat Moderate to Severe Ulcerative Colitis? – https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/uc-medicines
- Ulcerative Colitis – an overview – https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/ulcerative-colitis
- Ulcerative colitis: Recent advances in the understanding of disease pathogenesis – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7194476/
- Ulcerative Colitis in Adults—A Review – https://jamanetwork.com/journals/jama/fullarticle/2809412